
What Is Dialysis?

Why do people need dialysis?
If you have conditions like high blood pressure or diabetes, you are at higher risk for kidney failure, which means you may eventually require treatment like a kidney transplant or dialysis. Dialysis removes excess fluid from the body, helping to control blood pressure. Working with your doctor to keep blood sugar and blood pressure controlled may help keep your kidneys working longer.
Doctors use a number of kidney function tests to determine your kidney health. Most people begin dialysis treatment when they have a GFR of <15, meaning they’ve lost about 85 to 90 percent of their kidney function. Early diagnosis of CKD and regular monitoring can help you keep your kidneys functioning for as long as possible—and allow you and your doctor to plan for dialysis treatment or a preventative transplant when necessary.
What is dialysis: the facts at a glance
Dialysis is a treatment that can help you live well with ESRD.
- Dialysis can perform regular functions that your kidneys are no longer able to perform themselves.
- Dialysis helps to keep your body’s potassium, phosphorus, and sodium levels balanced.
- Dialysis empowers you to live a full, active life with kidney failure.
- There are two types of dialysis: hemodialysis and peritoneal dialysis.
- More and more people are choosing home dialysis, which can offer greater flexibility and better outcomes.
- The best dialysis option for you is the one that best fits your lifestyle and health needs.
- Many people switch dialysis treatment types to fit a changing lifestyle at some point during long-term treatment.

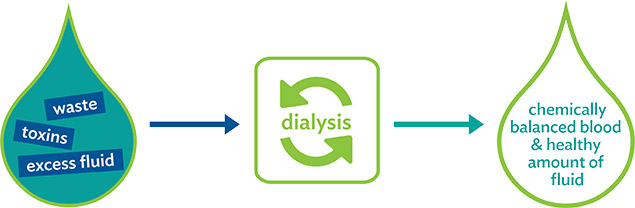
How does the dialysis process work?
Dialysis acts as an artificial kidney by filtering toxins, waste, and fluid from your blood through a semipermeable membrane—a material that allows fluids and small particles to flow through it, but not larger particles. The two types of dialysis, hemodialysis (HD) and peritoneal dialysis (PD), use different methods to filter toxins from your body. With HD, the filtering membrane is called a dialyzer and is a part of the dialysis machine. Your blood is circulated through the dialysis machine and cleaned before being returned to your body. With PD, the filtering membrane is the natural lining of your peritoneum or abdomen, and blood never leaves your body. Both types of dialysis also use a dialysate solution in the filtering process to help remove unwanted waste and toxins.
Comparing the two types of dialysis
Peritoneal dialysis
PD uses the blood vessels in the lining of your abdomen—the body’s natural filter—along with a solution called dialysate to filter toxins. With this method, a peritoneal catheter serves as your access into your abdomen and blood never leaves your body. Home peritoneal dialysis can be done with a machine or manually at home, at work, or even while traveling.Hemodialysis
HD filters your blood using a dialysis machine or through a dialyzer. Once you are connected to the machine via your hemodialysis access, blood flows into the machine, gets filtered, and is returned to your body. Hemodialysis is performed either at home or in a dialysis center. Home hemodialysis can be performed in the comfort of your own home, either with the help of a care partner or on your own. In-center hemodialysis is performed by a trained team of nurses and technicians.How long does dialysis take?
With PD, the length of treatment will depend on whether you choose continuous ambulatory peritoneal dialysis (CAPD) or automated peritoneal dialysis(APD):
- CAPD treatments are done manually, without a machine, about three to four times per day.
- APD uses a machine called a “cycler” and can be done as a longer single session while you sleep, as multiple shorter sessions during the day or night, or as a combination of these options.
With hemodialysis, your treatment length and frequency depend on your doctor’s prescription and where you receive your treatment:
- HD can be done five to six days a week for two and a half to three hours at a time, three days a week for three to five hours, or for six to eight hours while you sleep every night or every other night. You may also require longer treatments or a different weekly number of treatments, depending on your unique condition.
- In-center hemodialysis is typically done three times a week for three to four hours during the day or eight hours for nocturnal hemodialysis.
Dialysis treatment is most often prescribed by a nephrologist (kidney doctor). It’s important to start seeing a nephrologist as early as possible, so if you’re not already seeing one, talk to your doctor about getting a referral. Together, you and your nephrologist will discuss treatment options and determine what’s right for you.
When it’s time to start dialysis treatment, your nephrologist will prescribe your treatment time and frequency based on your unique health needs. It’s important to complete your dialysis treatment exactly as prescribed to feel your best.
Your treatment schedule is personalized to your exact needs. Completing every prescribed treatment will help you feel your best.


